This brief presents considerations for contextualising and responding to the mpox outbreak in the mining towns of South Kivu province in the Democratic Republic of the Congo (DRC). The brief focuses on women and children living and working in artisanal and small-scale mining (ASM) areas. Although mpox is endemic in certain provinces in the DRC, a nationwide outbreak of mpox (clade I) was declared in late 2022. In 2023, the number of confirmed cases of mpox in the DRC was the highest in Africa, with about 595 cases.1 A new strain was identified in Kamituga in September 2023, referred to as the new strain of clade I or clade Ib.2 This outbreak is characterised by widespread human-to-human transmission, unlike previous outbreaks which were primarily characterised by animal-to-human contact.3
In Équateur province in north-western DRC, most documented cases were in children, while in South Kivu in eastern DRC, cases were documented in women (including women who engage in transactional sex) and children under the age of 15, including newborns.4 The DRC Ministry of Public Health and Hygiene has approved two emergency mpox vaccines and is putting in place a series of preventive measures, starting with awareness and hygiene, in a context where many health districts lack timely access to diagnostics and vaccines.5
This brief highlights relevant socio-political contexts related to ASM, livelihoods, population mobility, and conflict and public health interventions. It discusses considerations for mpox vulnerabilities and access to healthcare for women and children. This brief draws on a SSHAP roundtable discussion on mpox in the DRC held in May 2024;6 conversations with experts and health actors active and/or knowledgeable in the region and outbreak; the authors’ own expertise on women’s and children’s lives in ASM areas in South Kivu; and academic and grey literature.
Key considerations
- Consider the heterogeneous and rapidly changing picture of mpox in DRC when identifying populations and interventions. Contextualise response plans to the socio-economic landscape in the mining towns in South Kivu province, including to shifts in transmission dynamics and spatial distribution of cases.
- Incorporate a detailed understanding of how local mining economies impact people’s vulnerability. Women working in mines face a range of intersecting health, economic and safety challenges. Understanding women’s livelihood strategies is critical to developing appropriate responses to mpox and to avoid inadvertently economically penalising women. For example, enforcing isolation measures or curtailing movements of suspected cases without considering social protection and loss of income could result in women and children potentially adopting risky mitigation strategies.
- Strengthen healthcare infrastructure in ASM areas and include gender-sensitive programmes. The ongoing mpox outbreak is revealing – and potentially exacerbating – structural barriers to access healthcare. For example, women represent a large proportion of workers in mines, and they may be less likely to have savings to pay for healthcare (for themselves and dependents) due to discriminatory employment patterns, which could hinder access to mpox diagnosis and care.
- Recognise and address the movement of people in mining areas across regions and borders to support their livelihoods in mpox preparedness plans and containment strategies. Securitisation and public health responses to mpox that curtail movement could harm vulnerable workers who are dependent on accessing commercial routes and corridors to survive. Mpox preparedness plans and containment strategies should therefore mitigate protection and surveillance risks at borders.
- Prioritise access to mpox detection and vaccination for pregnant women and children. Women and children in mining communities are particularly vulnerable to mpox. Women, who often handle food and care for children, are at risk of contracting the virus and spreading it within the household. Children and pregnant women are at risk of developing complications and death from mpox. Risk communication and community engagement campaigns should consider risks of stigmatisation when addressing vulnerability.
- Avoid stigmatising communities and social groups by associating them with the mpox virus. With the spillover of the virus in neighbouring countries, there is a danger of singling out specific groups. For public health measures to be effective and to foster social cohesion, it is important to avoid stigmatising communities and social groups associated with the mpox virus. Stigmatisation can lead to discrimination, avoidance of health services and increased isolation, thereby exacerbating the outbreak’s impact.
- Avoid the use of ‘sex worker’ when referring to populations at risk of mpox. Transactional sex dynamics need to be better understood in relation to women’s discrimination and poor working conditions in mines and in consideration of overall livelihood strategies. Greater understanding of women’s livelihood strategies in ASM – which can involve commercial sex and less visible forms of transactional sex – will inform appropriate and inclusive interventions.
- Incorporate a conflict-sensitive lens in all mpox responses in eastern DRC. Eastern DRC, and particularly South Kivu province, is characterised by ongoing conflict, social fragmentation and complex humanitarian needs. When responding to outbreaks like mpox, it is vital to incorporate a conflict-sensitive lens and rights-based approach to ensure that interventions do not exacerbate existing tensions and that the human rights of all individuals are upheld.
- Involve women and women-led associations in mpox responses. Involving women and women-led associations is essential for developing effective public health strategies for mpox that consider the unique needs and perspectives of women. There are women-led community-based organisations (CBOs) locally rooted and trusted by women in communities, which can act as socio-cultural navigators for national and international organisations rolling out mpox outbreak responses in ASM.
- Listen to children’s voices and engage them in mpox responses. Children in ASM zones face unique challenges and vulnerabilities. In addition to health, protection and physical dangers, they may also experience limited access to education, healthcare and other essential services. Children are at a high risk of developing complications from mpox. School-based and mine-based interventions targeting children should be explored, recognising that we need to better understand connections between child labour in mines and school attendance.
- Integrate mpox responses with health, protection and economic empowerment programmes for women and children in mines. Women in mines often face unique health risks and economic challenges, which can be exacerbated during health emergencies like mpox outbreaks. Community-based programmes that provide protective measures against mpox while promoting women’s economic independence can help mitigate the socio-economic impacts of the virus, ensuring that women are not only protected but also economically empowered during health crises.
New strain of mpox clade I in mining towns in South Kivu province
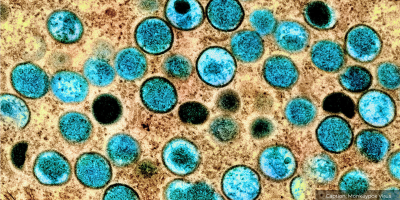
Mpox, a viral zoonotic disease, has emerged as a significant health concern in the DRC. Recent epidemiological reports indicate a high fatality rate amongst children aged 15 years and under.7,8 The reports also indicate that children and pregnant women are at risk of developing complications from mpox.5 More than 14,000 cases and 511 deaths have been recorded this year (as of August 2024), including women and children.9 The epidemiological dynamics of the new strain of the clade I mpox outbreak remain uncertain. However, evidence suggests it can affect anyone.10
In September 2023, a large mpox outbreak emerged in the town of Kamituga in South Kivu province, with high numbers of cases in ASM communities. In November 2023, the World Health Organization issued outbreak news of the first cases of sexually transmitted clade I mpox virus in the DRC.11 The genome of samples from Kamituga revealed a mutated strain of mpox, referred to as the new strain of clade I or clade Ib. The disease is transmitted to humans through contact with infected animals or contaminated materials, and human-to-human transmission can occur through respiratory droplets, bodily fluids and skin lesions.1 The virus has spread to Goma, the capital city of North Kivu province, including in crowded camps where displaced populations reside, and has now been identified in neighbouring countries. The outbreak was declared a public health emergency of continental security on 13 August 2024 by Africa CDC,12 and a public health emergency of international concern by the WHO Director-General on 14 August 2024.13
In mining areas, key populations have been identified in public health interventions and health promotion campaigns as particularly at risk of contamination and of spreading the mpox virus.14 These populations include men who have sex with men, sex workers, and migrants. The prevalence of HIV is higher in the eastern provinces of the DRC than in the rest of the country, where access to antiretroviral treatment is often challenging, putting people with HIV at higher risk of severe mpox and death, if infected.5 The complex dynamics of transactional sex, gender and livelihood opportunities for women in mines are often overlooked by public health narratives of vulnerability, which tend to isolate transactional sex from its broader socio-economic context.
The socio-political context of eastern DRC
Entrenched conflicts in eastern DRC and the insecurity characterising many areas in South Kivu intersect with efforts to implement public health interventions, including outbreak responses in mining communities.
Conflict dynamics in the DRC
Conflict, instability and resource exploitation. Eastern DRC has experienced decades of armed conflict, fuelled by intercommunal tensions, land disputes, competition over natural resources, power struggles and failed national and international peacebuilding strategies.15 This has resulted in a sustained and fragmented presence of various armed groups and militias.15 Protracted violence has led to widespread human rights abuses, displacement of populations, loss of livelihoods and a breakdown of governance structures. The DRC is rich in natural resources, including gold, coltan (columbite-tantalite), cobalt and other minerals, which have attracted both domestic and foreign interests. The exploitation of these resources has been a driving force behind the conflict in the region, as armed groups seek to control mining areas and profit from the illicit trade of minerals.16 This has perpetuated a cycle of violence and instability, further exacerbating the socio-political challenges faced by the population of eastern DRC. The weak governance structures and lack of effective rule of law in the region have also contributed to the socio-political complexities of eastern DRC. Furthermore, the insecure context has led humanitarian agencies to stop or suspend their activities on occasions.17
Corruption, impunity and a lack of accountability. Efforts to address the root causes of conflict and instability have been undermined by corruption, impunity and a lack of accountability.18 The conflicts are compounded by ongoing humanitarian crises, which exacerbate tensions and provoke large-scale displacement; widespread poverty; and persistent socio-economic inequalities. The population of eastern DRC continues to face challenges related to accessing basic services, such as healthcare and education, as well as protection from human rights abuses. Challenges to accessing healthcare in eastern DRC are worsened by socio-political underlying causes of conflict and instability. Learning from the Ebola outbreaks in the DRC tells us that human rights and social protection considerations shape the dynamics of outbreaks. It is therefore critical to design appropriate responses from a human rights perspective.19
Cross-border mobility
Complex migration patterns. Large numbers of people are moving between eastern DRC and neighbouring countries, such as Rwanda, Burundi and Uganda, where mpox cases have now been confirmed.9 There are many reasons why people move across these borders, including for trade and employment opportunities, because they are displaced by natural disasters or to migrate internally and/or cross borders in search of protection.20 Mining-related mobility in eastern DRC is also highly heterogeneous, with women and men turning to ASM due to losses of land and agricultural livelihoods; to seek economic opportunities; and in search of a safe place.21 Alongside refugee camps, people on the move are being hosted by friends and relatives.22 Women engaging in commercial and transactional sex in South Kivu may be from neighbouring countries, and – like other mine workers – they are often highly mobile.6
Efforts to address mpox in South Kivu and cross-border implications. International organisations, including the World Health Organization and the Centers for Disease Control and Prevention, have collaborated with national health authorities to strengthen surveillance systems, enhance diagnostic capabilities and improve outbreak response mechanisms.23 The International Organization for Migration has also committed support for surveillance and risk communication at border sites, points of entrance and along mobility corridors.24 Vaccination campaigns targeting at-risk populations and health education initiatives aimed at raising awareness about mpox transmission and prevention have also been crucial components of these efforts. Such prevention and containment initiatives must protect groups labelled as spreading the virus (such as commercial sex workers, men who have sex with men, or truck drivers), to avoid reproducing discourses of blame. Furthermore, regional cooperation and coordination among neighbouring countries are essential to develop a unified approach to mpox prevention and control. Experiences from Ebola and COVID-19 in the DRC show that communities can perceive the militarised enforcement of public health responses negatively.3
Cross-border disease management initiatives. Cross-border surveillance, information sharing and joint response exercises are instrumental in containing outbreaks and preventing further spread of the disease across borders. The ongoing conflict and instability in South Kivu, coupled with socio-economic factors, such as poverty and limited access to healthcare, continue to hamper disease control efforts and resilience-building initiatives. The International Organization for Migration and the DRC Ministry of Public Health and Hygiene conducted participatory mapping of population mobility to understand the mobility dynamics of the spread of zoonotic diseases, such as the mpox virus. The mapping highlighted commercial connections between ‘the epicentre’ and the main cities of South Kivu (Bukavu and Uvira) and North Kivu (Goma); and the neighbouring countries of Burundi and Rwanda.24 It is therefore crucial to understand the local and transnational ecosystem surrounding ASM activities in eastern DRC, including the roles and mobility of women and children, to ensure that responses to contain mpox outbreaks do not exacerbate economic vulnerabilities and stigma.
Implications for mpox responses
The protracted armed conflict in eastern DRC is severely impeding access to health services for residents. The uncertainty that violence brings to local communities has profound implications on outbreak responses.25 Evidence shows that the socio-economic lives of migrants, refugees and internally displaced people can be highly impacted by public health measures during epidemics.26 For example, during the COVID-19 pandemic, domestic workers living in camps lost their jobs and turned to risky alternative livelihood strategies, such as transactional sex and child labour.27 Measures implemented during the COVID-19 pandemic also created legal and social insecurities for migrants. Responses to mpox must therefore consider the diverse population in eastern DRC and attend to legal and socio-economic vulnerabilities. Experiences from COVID-19 suggest that risks-based approaches should be prioritised over closing borders to protect people’s livelihoods. The movement of populations and armed groups also increases risks for cross-border mpox transmission.25 Eastern DRC is a highly militarised region and has recently gone through a fragmentation of armed groups. Responses led or supported by the army or non-state actors may be associated with geopolitical tensions and trigger community suspicion, with a potential longer-term detrimental effect on trust towards health services. Box 1 offers an example of guidelines developed by CDA Collaborative Learning to include conflict-sensitive approaches in public health programmes.28
Box 1. Adapting public health programmes for conflict sensitivity: Frameworks developed by CDA Collaborative Learning28
| ‘It is clear that many public health initiatives recognize the need to take conflict sensitivity into account. The question is: how? The following section outlines a process to take public health practitioners through the steps of a basic Do No Harm analysis. It is important that this process involves stakeholders who have significant experience in and diverse perspectives on the communities at the heart of the analysis. It is also important to remember that conflicts, public health emergencies, and humanitarian crises are dynamic and that there may be a need to revisit and adapt different steps of this process as the situation evolves.
1. Map out conflicts in the areas where you are working. This includes the gender and identity dynamics of the conflict. Remember that there is often more than one conflict happening at any given time. You can then map out the impacts of the conflict on public health, again paying attention to underlying gender and identity dynamics. 2. Develop a list of Dividers and Connectors in your intervention areas. Be as specific as possible […] 3. Describe your programs, in-depth, as they are currently planned. This includes: what you intend to do; how you intend to carry it out; who is involved in the process; who is receiving goods and services; when and where those goods and services are being organized; and a brief summary of the logic behind those decisions. 4. For each Divider and Connector, assess whether and how your program (and the broader public health crisis) could affect it. This process often involves thinking through both best-case and worst-case scenarios. It is therefore important to write down all the potential effects, even if unlikely. This is essentially a brainstorming phase; you can prioritize the most likely effects in the next step. 5. For each instance where your program or actions may weaken a Connector or strengthen a Divider, generate options that can prevent or mitigate that potential negative effect. If there are a lot of Dividers and Connectors, it may be helpful to prioritize and focus on the Dividers or Connectors most likely to have a significant impact on the population and/or those over which the organization has greater control. 6. Assess whether and how organizational patterns and staff behavior may affect conflict and public health response dynamics. Identify whether the program has any vulnerability to theft or the potential to affect markets and/or local authorities (whether formal or informal). Then identify the effects these circumstances might have on conflict dynamics and the public health response, and generate options to mitigate any negative impact. Think through how staff behavior might affect conflict dynamics, and generate checklists of behavior to prevent, reduce, or mitigate those risks.’ |
Source: Conflict Sensitivity & Public Health Emergencies: Practical programming adaptation during COVID-19 and beyond. Cambridge, MA: CDA Collaborative Learning Projects, October 2020, p.15.
Examples of ‘dividers’ (factors that create division or tension) and ‘connectors’ (factors that promote cohesion and coexistence) listed in the guidelines developed by CDA Collaborative Learning include: systems and institutions; attitudes and actions; values and interests; symbols and occasions; and experiences (for example, experiences of distrust are dividers while lessons learnt from responding to an outbreak can constitute a connector).28 Dialogue-based initiatives with different groups can help develop various understandings of mpox and perceived connexions with conflict dynamics.3
The ASM landscape in South Kivu
ASM areas in South Kivu, where mpox transmission has been documented, play a significant role in the local economy, social dynamics and environmental sustainability in eastern DRC.
The political economy of ASM
ASM represents a complex and often contentious sector. The ASM sector revolves mainly around the extraction of minerals, such as gold, tin, tantalum, tungsten and coltan.29 These minerals are essential components in various industries, including electronics, automotive and aerospace, making them valuable commodities in the global market. However, the extraction process in the ASM sector is characterised by informal practices, minimal mechanisation and often rudimentary technology,30 leading to significant environmental degradation and social challenges.
ASM provides livelihoods in South Kivu. Economically, the ASM sector provides livelihoods for a substantial portion of the local population in South Kivu, particularly in rural and resource-rich areas where there are limited formal employment opportunities. Artisanal miners, known as ‘creuseurs’, work independently or in small groups, often under precarious conditions and with little to no legal or regulatory oversight. The income generated from ASM activities supports not only miners and their families but also local businesses that provide goods and services to support mining operations.
Working conditions in ASM
Exploitation cycles in the informal sector. Child labour, unsafe working conditions and exploitation by intermediaries and armed groups who control mining territories have been documented in ASM mines,30 and little is known about the extent to which children might be drawn into transactional sex. Moreover, fluctuating mineral prices and lack of access to the market often leave miners vulnerable to poverty and economic instability. Socially, the ASM sector in South Kivu has contributed to the proliferation of informal networks and power dynamics that influence local governance and conflict dynamics.
Social and political tensions. Competition over mining sites and control of mineral revenues have been linked to instances of violence and instability, exacerbating existing tensions in the region. Moreover, the influx of miners from different ethnic and regional backgrounds has sometimes strained social cohesion, leading to intercommunal conflicts over land and resources. Environmentally, the ASM sector in South Kivu has significant negative impacts, including deforestation, soil erosion, water contamination and loss of biodiversity. The use of mercury and other toxic chemicals in mineral processing poses risks to both miners and biodiversity.
Women’s livelihoods in Kamituga’s ASM sector
The mining region in Kamituga is a significant source of livelihood for many people, including women. Despite the economic opportunities, women in Kamituga’s mining region face challenges that impact their livelihoods.
Women’s roles in Kamituga’s ASM sector
Women’s roles in mining-related activities. Women participate in various aspects of the mining industry – from extraction and processing to trading – as well as in mining-related activities, such as hospitality, petty trade and sex work. Women’s participation is crucial for the local economy, as they contribute significantly to household income and community development. Women often engage in ASM, which is labour-intensive and requires minimal technological input. Kamituga provides a relatively accessible means of earning a livelihood, especially for those with limited education and resources.31 The DRC’s socio-economic situation, discriminatory mining governance and patriarchal heritage mean that many women in mining areas are drawn into transactional sex, either for work or to supplement their income and feed their families. Researchers speak of pathways of economic interdependence and partnerships between men and women in the mining site.32 However, for some women working in mining areas, sex is used for material and financial benefit and contributes to their livelihood, leading to a tendency to sexual services. The dynamics of transactional sex do not only affect single women.33
Discrimination and gender bias. Despite their recognised contributions, women in Kamituga’s mining sites face challenges that hinder their economic empowerment and overall well-being.34 Women often face discrimination and gender bias in the mining region. They are typically assigned lower-paying and more labour-intensive tasks than their male counterparts. This gender disparity is rooted in deep-seated cultural norms and societal expectations that undervalue women’s work.35
Sexual harassment and violence. Sexual harassment and violence are pervasive issues in the mining region. Women miners are frequently subjected to harassment by their male colleagues and superiors, creating a hostile and unsafe working environment.36 This not only affects their mental and physical health but also limits their ability to work effectively and earn a stable income.
Lack of access to resources and training. Women in the mining region often lack access to essential resources, such as credit, equipment and training. This limits their ability to improve their mining techniques, increase their productivity and enhance their earnings. The absence of formal training programmes also means that women are less likely to adopt safer and more efficient mining practices.
Health risks. The mining environment poses significant health risks due to hazardous chemicals, dust, and physically demanding labour. Women – who often work without adequate protective equipment – are particularly vulnerable to these hazards and face increased risk of miscarriage and communicable diseases, such as tuberculosis, urinary tract infections, HIV and other sexually transmitted diseases.37 Additionally, the scarcity of healthcare facilities and health insurance further exacerbates the impact of these risks on their well-being. In some artisanal mining sites, there are reports of women being asked to carry a ‘yellow card’, which guarantees that they have been tested negative for HIV and therefore allows them to live and work on the site. This is an indication of practices that violate human rights and increase discrimination against women.
Economic exploitation. Women miners are often economically exploited by intermediaries who purchase their minerals at unfairly low prices. This exploitation is facilitated by the lack of market information and bargaining power among women miners, further entrenching their economic vulnerability.36
Implications for mpox responses
Women in Kamituga’s ASM areas play a vital role in the local economy. They are involved in a wide range of mining-related activities, often making a significant contribution to the household’s income. Yet they face challenges rooted in discrimination that undermine their livelihoods and their health. Mpox responses require a comprehensive approach, integrating strategies to promote gender equality (equal rights and opportunities) and equity (fairness in treatment); and non-exploitative employment; ensure safety; enhance access to resources; and strengthen market access. Economic empowerment and social protection promoting gender equity and autonomy are intertwined with improved access to health services.
Women are often aware of the short-term and long-term health risks associated with living on mining sites for themselves and their children.38 They turn to ASM as a last resort livelihood strategy. Mpox responses (including risk communication and community engagement (RCCE) strategies) should include clear information regarding pathways, advice and support on how to access healthcare for mpox. These should consider women’s working schedules.
Mpox responses in ASM areas have been particularly concerned with women labelled by policies and programmes as ‘sex workers’. The realities of gender dynamics and structural discriminations mean that a wider range of women engage in transactional sex. The label of ‘sex worker’ therefore does not capture the full picture and can also further stigmatise categories of women by associating them with mpox. Understanding the livelihood strategies developed by women over time is critical to protect them from mpox and contain the virus.
Healthcare for women and children in mining communities
Between 28 September 2023 and 3 March 2024, South Kivu province recorded almost 229 laboratory-confirmed cases, with the highest number of cases in Kamituga.8 Mining activities are a significant source of livelihood for many families.30 However, these activities can also create numerous health challenges, especially for women and children. Access to healthcare in mining communities is often limited, exacerbating the health risks associated with mining activities.8 Women and children in mining communities are most often involved in farming and looking after small livestock around the house. Such close contact with animals, combined with poor living conditions, make them particularly vulnerable to mpox. Women, who often handle food and care for children, are at risk of contracting the virus and spreading it within the household. In addition to close contact with animals, vulnerability is increased by person-to-person contact. Given the proximity of interaction in women’s workplaces, such as markets and churches, women are at higher risk of community transmission. Women are also at risk of sexual transmission given the high prevalence of transactional sex in these areas. Furthermore, there is a risk of vertical transmission, where mothers can pass the infection to their children with potentially severe consequences.39
Health risks for women and children in ASM sites
Mining activities pose health risks due to exposure to hazardous substances, poor working conditions and inadequate healthcare infrastructure. Women and children are particularly vulnerable to these risks for several reasons.
Exposure to hazardous substances. Mining operations often involve the use of toxic chemicals, such as mercury and cyanide, which can contaminate water sources and soil. Women, who work in processing minerals, and children, who play near mining sites, are at high risk of exposure to these harmful substances. Prolonged exposure can lead to severe health issues, including respiratory problems, skin diseases and neurological disorders. Involving children in mining without any protection exposes them to serious illnesses,30 which can even lead to early death.
Poor working conditions. Women working in the mining sector often face harsh working conditions, including long hours, heavy physical labour and inadequate protective equipment. These conditions can lead to chronic health problems, including musculoskeletal disorders and reproductive health issues.
Inadequate healthcare infrastructure. Mining communities, particularly in remote areas, often lack adequate healthcare facilities. This makes it difficult for women and children to access essential medical services, including maternal and child healthcare, vaccinations and treatment for common illnesses. Kamituga is a very isolated mining town. This location limits the humanitarian aid available to make up for the lack of government assistance. In ASM, people also turn to the private sector for healthcare and use their own resources, savings or communal strategies to pay for medical treatment.40
Information, healthcare access and treatment. There is often limited awareness about mpox and its prevention in mining communities. The symptoms of mpox, including fever, rash and swollen lymph nodes, require prompt medical attention. However, limited healthcare facilities and limited resources in mining areas make diagnosing and treating the disease difficult. This leads to severe complications and increased mortality rates, particularly among children.10
Children in mining communities
Poverty and lack of access to healthcare. In ASM sites, children may be exploited for child labour as a result of factors including economic hardship, lack of educational opportunities and the country’s history of conflict and instability. Poverty plays a significant role in driving children to work in mining sites in the DRC.41 Many families living in poverty rely on the income generated by their children working in mines to survive.30,41 The lack of alternative sources of income and limited access to education further exacerbate the problem, trapping children in a cycle of exploitation. Moreover, the mining sector’s healthcare system is severely underfunded and lacks adequate resources to provide essential services to the population.42 Children working in mining sites are often exposed to hazardous working conditions, including exposure to toxic chemicals and physical dangers.43 The lack of access to healthcare means that these children are at a higher risk of injuries, illnesses and long-term health consequences. Insecurity caused by armed groups is exacerbating the situation.44 Mpox has added to the vulnerability of children already living in extreme poverty.
Susceptibility to disease, respiratory issues and malnutrition. Children living in mining communities are more susceptible to infectious diseases, respiratory issues, skin diseases and malnutrition,42 all of which heighten their vulnerability to illnesses like mpox. Children in mines often miss their vaccinations, putting them at high risk of several vaccine preventable diseases. This poses challenges for adherence to future mpox vaccination. Working conditions in the ASM sector are unfavourable for young children, with adverse effects on their long-term health.42 Women’s vulnerability to mpox in mines can also affect children. Mpox can be transmitted to the foetus during and after pregnancy. Miscarriages and stillbirths have been reported amongst confirmed mpox cases during pregnancy.39
Interconnection between vulnerability at school and in mining sites. Mpox is a highly contagious viral disease that can spread rapidly in crowded environments, such as schools and mining sites. The transmission of mpox occurs primarily through respiratory droplets expelled when an infected person coughs or sneezes, as well as through direct contact with infected skin lesions. In settings where individuals are in close proximity to one another, such as schools and mining sites, the risk of mpox transmission is heightened.8 The transmission of mpox between children working in mines and in schools creates a vicious circle of infection. Children working in mines may bring the disease back to their communities, including schools, where it can spread among their peers. Conversely, infected schoolchildren may introduce mpox into mining communities. Following preventive measures and raising awareness about mpox transmission can help reduce the risk of the disease spreading among children at school and individuals on mining sites. To prevent the transmission of mpox in these settings, it is also crucial to implement strict infection control measures. These include promoting good hygiene practices, such as handwashing with soap and water, covering coughs and sneezes, and avoiding close contact with individuals who are sick.
Box 2. How to engage children: Guiding principles and processes developed by SSHAP45
‘All levels of child engagement should follow basic ethical principles. Operating in the best interest of the child forms the basis for all child engagement. This means that engagement should always prioritise children’s needs and rights. The following considerations are important when engaging children at any level of participation:
|
Source: Reilly, E., Serlemitsos, E. and Bilakwate, J. (2024). Key Considerations: Child Engagement in the Context of Disease Outbreaks in Eastern and Southern Africa. Social Science in Humanitarian Action (SSHAP), p.9–10.
Implications for mpox responses
Entrenched inequalities and health risks associated with living and working conditions in ASM areas heighten the vulnerability of women and children to mpox. Given the weak health infrastructure in ASM areas in South Kivu, community education programmes are essential to raise awareness about mpox and promote preventive measures, such as hygiene practices, safe handling of animals and the importance of seeking medical care for symptoms of infectious diseases.
Working mothers are often forced to bring their young children to the mining sites, due to a lack of childcare alternatives. Meanwhile, entrenched poverty may push children to work in mines and drop out of school to supplement family incomes. It is important that mpox RCCE programmes also target children directly (see Box 2).
Holistic interventions, combining measures that target mpox with broader protection and economic and social protection programmes, are therefore required to respond to the health needs of women and children. Interventions aimed at containing the virus, including mandatory hospitalisation for positive cases,46 can increase the precarity of miners’ livelihoods. Further, the isolation or threat of isolation present additional challenges for women in ASM sites who are caring for children, which could influence women’s willingness to be tested.
Promoting participatory approaches
Women are often involved in outbreak responses because they play critical roles in community health, from caregiving to disseminating information. In ASM, women also contribute significantly to their household’s income and are often the primary family breadwinners, and are involved in a wide range of organisations and associations.
Collaborate with women-led organisations
The response to mpox outbreaks can benefit significantly from collaborating with women-led associations. Women-led associations are integral to the social fabric and community resilience and can play a crucial role in the local community, offering a foundation for effectively implementing responses to health crises like mpox. These organisations range from women’s mining cooperatives to human rights organisations. Examples include Association de Lutte contre les violences sur les Enfants et les Femmes dans les Mines (ALEFEM), Initiative d’Appui Social et intégral des Femmes et des enfants (IASFM), Association des Mamans Bizalu de Kamituga (AMBIKA) and Mutuelle de Solidarité des Mamans Loutra (MUSOMAL).
Women are actively involved in the non-governmental organisation sector in Kamituga. The social fabric of women’s involvement in public affairs can be leveraged for mpox responses, including to develop gender-responsive approaches that empower women to participate in decision-making processes and health interventions.47
Women-led organisations often function as hubs for social support, information dissemination and collective action in response to various challenges, including health emergencies. As the President of IASFM, Mrs Emilienne Itongwa told us:
‘When a woman has a problem, she or one of the cooperative managers calls us and we can see how we can advocate on her behalf. Things have changed considerably nowadays. Before, women were very badly treated… For example, in the event of disputes between the digger and the gravel mom or the twangeuse, they were beaten up and sometimes touched (even intimately) in search of a supposedly stolen mineral.’48
These organisations are therefore the first point of contact with women in the mines (living in and around the sites). The organisations also provide a platform where women can make their voices heard and their problems identified. In the context of epidemics, such as mpox, it is essential to know and understand the vulnerability of women in the mines, especially given the dynamics of transactional sex, which is often not visible nor spoken about. In the context of the ongoing mpox outbreak, women-led CBOs can act as a first point of contact for information on mpox for vulnerable or marginalised people who may be afraid to seek help in health centres. They can also act as socio-cultural navigators to help national and international organisations implementing outbreak responses adopt appropriate ways to approach and diagnose women and children and offer treatment.
Tailored engagement with women, including pregnant women, is also key when planning for mpox vaccination campaigns, as vaccination of children and potentially pregnant women may elicit anxiety.3
Prioritise local involvement
Promoting participatory approaches to combat mpox in the ASM sector is crucial for fostering community ownership and access to healthcare. Engaging local miners and their families in the design and implementation of health strategies ensures that the responses are culturally relevant and specific to the context.49 By prioritising local involvement, mpox responses can be more effective and sustainable, ultimately reducing the spread of mpox and improving health outcomes in vulnerable mining areas, such as Kamituga. In the mining towns of South Kivu, mpox responses must include actions to meet the health needs and promote the protection of people engaging in transactional sex.50 Lessons can be learnt from HIV peer-led approaches with women engaging in commercial and transactional sex through CBOs active in areas where key populations are present and risks are high – such as truck stops, bars or short-term guest houses.51 Working with women engaging in transactional sex through broader community empowerment programmes can reduce risks of harmful stigmatisation.
References
- Mercy, K., Tibebu, B., Fallah, M., Faria, N. R., Ndembi, N., & Tebeje, Y. K. (2024). Mpox continues to spread in Africa and threatens global health security. Nature Medicine, 30(5), 1225–1226. https://doi.org/10.1038/s41591-024-02862-6
- Masirika, L. M., Nieuwenhuijse, D. F., Ndishimye, P., Udahemuka, J. C., Steeven, B. K., Gisèle, N. B., Musabyimana, J. P., Daniel, B. N., Kiluba, T. K. wa, Mweshi, F. K., Ngabo, P., Tambala, T., Divin, M. M., Chance, B. M., Mambo, L. M., Schuele, L., Mbiribindi, J. B., Martinez, G. S., Kelvin, D. J., … Siangoli, F. B. (2024). Mapping the distribution and describing the first cases from an ongoing outbreak of a New Strain of mpox in South Kivu, Eastern Democratic Republic of Congo between September 2023 to April 2024 (p. 2024.05.10.24307057). medRxiv. https://doi.org/10.1101/2024.05.10.24307057
- Hrynick, T., Muzalia, G., & James, M. (2024). Key Considerations: Risk Communication and Community Engagement for Mpox Vaccination in Eastern DRC. Institute of Development Studies. https://doi.org/10.19088/SSHAP.2024.024
- European Centre for Disease Prevention and Control. (2024, April 5). Outbreak of mpox caused by Monkeypox virus clade I in the Democratic Republic of the Congo. https://www.ecdc.europa.eu/en/news-events/outbreak-mpox-caused-monkeypox-virus-clade-i-democratic-republic-congo
- WHO. (2024, June 14). Mpox—Democratic Republic of the Congo. Disease Outbreak News. https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON522
- Hrynick, T., & Schmidt-Sane, M. (2024). Roundtable Report: Discussion on mpox in DRC and Social Science Considerations for Operational Response. Institute of Development Studies. https://doi.org/10.19088/SSHAP.2024.014
- WHO. (2024). Multi-country outbreak of mpox (No. 33; External Situation Report). WHO. https://www.who.int/publications/m/item/multi-country-outbreak-of-mpox–external-situation-report-33–31-may-2024
- Katoto, P. D., Muttamba, W., Bahizire, E., Malembaka, E. B., Bosa, H. K., Kazadi, D. M., Lubambo, G., Siangoli, F. B., Bakamutumaho, B., Wayengera, M., Landu, D. J. M., Mukadi-Bamuleka, D., Mbala, P., Loeb, M., Kirenga, B., & Muyembe-Tamfum, J.-J. (2024). Shifting transmission patterns of human mpox in South Kivu, DR Congo. The Lancet Infectious Diseases, 24(6), e354–e355. https://doi.org/10.1016/S1473-3099(24)00287-1
- UN. (2024, August 8). L’OMS s’inquiète d’une hausse sans précédent des cas de mpox en Afrique | ONU Info. UN. https://news.un.org/fr/story/2024/08/1147756
- WHO. (2023, December 11). Mpox (monkeypox). WHO. https://www.who.int/news-room/questions-and-answers/item/monkeypox
- WHO. (2023, November 23). Mpox (monkeypox)—Democratic Republic of the Congo. Disease Outbreak News. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON493
- Africa CDC. (2024, August 13). Africa CDC Declares Mpox A Public Health Emergency of Continental Security, Mobilizing Resources Across the Continent. Africa CDC. https://africacdc.org/news-item/africa-cdc-declares-mpox-a-public-health-emergency-of-continental-security-mobilizing-resources-across-the-continent/
- WHO. (2024, August 14). WHO Director-General declares mpox outbreak a public health emergency of international concern. WHO. https://www.who.int/news/item/14-08-2024-who-director-general-declares-mpox-outbreak-a-public-health-emergency-of-international-concern
- Vakaniaki, E. H., Kacita, C., Kinganda-Lusamaki, E., O’Toole, Á., Wawina-Bokalanga, T., Mukadi-Bamuleka, D., Amuri-Aziza, A., Malyamungu-Bubala, N., Mweshi-Kumbana, F., Mutimbwa-Mambo, L., Belesi-Siangoli, F., Mujula, Y., Parker, E., Muswamba-Kayembe, P.-C., Nundu, S. S., Lushima, R. S., Makangara-Cigolo, J.-C., Mulopo-Mukanya, N., Pukuta-Simbu, E., … Mbala-Kingebeni, P. (2024). Sustained human outbreak of a new MPXV clade I lineage in eastern Democratic Republic of the Congo. Nature Medicine. https://doi.org/10.1038/s41591-024-03130-3
- Vlassenroot, K., & Verweijen, J. (2017). 6 Democratic Republic of Congo: The Democratization of Militarized Politics. In M. Bøås & K. C. Dunn (Eds.), Africas Insurgents (pp. 99–118). Lynne Rienner Publishers. https://doi.org/10.1515/9781626376526-007
- Hanai, K. (2021). Conflict minerals regulation and mechanism changes in the DR Congo. Resources Policy, 74, 102394. https://doi.org/10.1016/j.resourpol.2021.102394
- MSF. (2024, May 24). DRC: Civilians caught in crossfire in North and South Kivu [Interview]. MSF. https://www.msf.org/drc-civilians-caught-crossfire-north-and-south-kivu
- Anderson, P. (2023). Cobalt and Corruption: The Influence of Multinational Firms and Foreign States on the Democratic Republic of the Congo. Journal for Global Business and Community, 14(1). https://doi.org/10.56020/001c.72664
- Kroll, G., & Gallego-Ayala, J. (2023, January 5). The social response to Ebola in DRC: Five recommendations for successful community engagement in emergencies. Development for Peace. https://blogs.worldbank.org/en/dev4peace/social-response-ebola-drc-five-recommendations-successful-community-engagement
- UNHCR. (n.d.). Democratic Republic of the Congo situation. UNHCR Global Focus. https://reporting.unhcr.org/operational/situations/democratic-republic-congo-situation
- Bashwira, M.-R., & Van Der Haar, G. (2020). Necessity or choice: Women’s migration to artisanal mining regions in eastern DRC. Canadian Journal of African Studies / Revue Canadienne Des Études Africaines, 54(1), 79–99. https://doi.org/10.1080/00083968.2019.1674170
- Sengenya, C. M. (2024, April 11). For Congolese displaced by the M23 war, host families offer a ‘heart of solidarity.’ The New Humanitarian. https://www.thenewhumanitarian.org/news-feature/2024/04/11/congolese-displaced-m23-war-host-families-offer-heart-solidarity
- WHO. (2022). Risk communication and community engagement (RCCE) for mpox outbreaks: Interim guidance,. WHO. https://www.who.int/publications/i/item/WHO-MPX-RCCE-2022.1
- IOM. (2024, June 5). IOM Expands Support to the Mpox Outbreak Response in DRC. IOM. https://ropretoria.iom.int/news/iom-expands-support-mpox-outbreak-response-drc
- Kavulikirwa, O. K. (2024). Intersecting realities: Exploring the nexus between armed conflicts in eastern Democratic Republic of the Congo and Global Health. One Health, 19, 100849. https://doi.org/10.1016/j.onehlt.2024.100849
- Duclos, D., & Palmer, J. (2020). Background Paper: COVID-19 in the Context of Forced Displacement: Perspectives from the Middle East and East Africa. Social Science in Humanitarian Action (SSHAP). https://www.socialscienceinaction.org/resources/background-paper-covid-19-and-forced-displacement-in-the-middle-east-and-east-africa/
- Hintermeier, M., Gottlieb, N., Rohleder, S., Oppenberg, J., Baroudi, M., Pernitez-Agan, S., Lopez, J., Flores, S., Mohsenpour, A., Wickramage, K., & Bozorgmehr, K. (2024). COVID-19 among migrants, refugees, and internally displaced persons: Systematic review, meta-analysis and qualitative synthesis of the global empirical literature. eClinicalMedicine, 102698. https://doi.org/10.1016/j.eclinm.2024.102698
- Conflict Sensitivity & Public Health Emergencies: Practical Programming Adaptation during COVID-19 and Beyond. (2020). CDA Collaborative Learning Projects.
- Kamundala Byemba, G., & Ndungu Mukasa, A. (2017). Etude de base sur la situation socio-économique des ménages vivant dans et autour des sites miniers au Sud-Kivu. CEGEMI, GIZ GmbH. http://cegemi.com/wp-content/uploads/2017/11/Kamundala-et-Ndungu-GIZ-2017_Etude-de-base-sur-la-situation-socio-%C3%A9conomique-des-m%C3%A9nages-vivant-dans-et-autour-des-sites-miniers-du-Sud-Kivu.pdf
- Murhi Mihigo, I., Vermeylen, G., & Munguakonkwa, B. (2024). Does the education system matter? Exploring in-depth joint school attendance, hazardous and non-hazardous activities in artisanal and small-scale mining in the Democratic Republic of the Congo. Heliyon, 10(10), e30771. https://doi.org/10.1016/j.heliyon.2024.e30771
- Byemba, G. K. (2020). Formalization of artisanal and small-scale mining in eastern Democratic Republic of the Congo: An opportunity for women in the new tin, tantalum, tungsten and gold (3TG) supply chain? The Extractive Industries and Society, 7(2), 420–427. https://doi.org/10.1016/j.exis.2020.03.001
- Bryceson, D. F., Jønsson, J. B., & Verbrugge, H. (2014). For Richer, for Poorer: Marriage and Casualized Sex in East African Artisanal Mining Settlements. Development and Change, 45(1), 79–104. https://doi.org/10.1111/dech.12067
- Bashwira Nyenyezi, M. R. (2017). Navigating obstacles, opportunities and reforms: Women’s lives and livelihoods in artisanal mining communities in eastern DRC [Wageningen University]. https://doi.org/10.18174/413901
- Kamundala, G., Marysse, S., & Iragi, F. (2014). Viabilité économique de l’exploitation artisanale de l’or au Sud-Kivu face à la compétition des entreprises minières internationales. Conjonctures Congolaises, 167–195.
- Rutherford, B., & Buss, D. (2022). The (In)Visibility of Women and Mining: The Gendering of Artisanal and Small-Scale Mining in Sub-Saharan Africa (1st ed.). Routledge. https://doi.org/10.4324/9781003245414
- Iguma Wakenge, C., Bashwira Nyenyezi, M.-R., Bergh, S. I., & Cuvelier, J. (2021). From ‘conflict minerals’ to peace? Reviewing mining reforms, gender, and state performance in eastern Democratic Republic of Congo. The Extractive Industries and Society, 8(2), 100894. https://doi.org/10.1016/j.exis.2021.100894
- Geenen, Sara & Bikubanya, Divin-Luc & Dunia Kabunga, Philippe & Igugu, Olivier & Kabilambali, Gracia & Katoto, Patrick & Marijsse, Simon & Mayeri, Daniel & Muhanzi Aganze, Gabriel & Mukotanyi Mugisho. (2021). La fièvre de l’or: Santé et environnement dans les mines d’or de Kamituga, RDC. Universiteit Antwerpen, 10. https://ideas.repec.org/p/iob/wpaper/2021.10.html
- World Vision. (2013). Child miners speak—Key findings on children and artisanal mining in Kambove DRC. World Vision. https://reliefweb.int/report/democratic-republic-congo/child-miners-speak-key-findings-children-and-artisanal-mining
- CDC. (2024, June 11). Clinical Considerations for Mpox in People Who are Pregnant or Breastfeeding | Mpox | Poxvirus | CDC. https://www.cdc.gov/poxvirus/mpox/clinicians/pregnancy.html
- Irenge, C. A., Bushenyula, P. K., Irenge, E. B., & Coppieters, Y. (2023). Participative epidemiology and prevention pathway of health risks associated with artisanal mines in Luhihi area, DR Congo. BMC Public Health, 23(1), 121. https://doi.org/10.1186/s12889-023-15020-3
- Godelive, K. B., Martin, D., & Nene, M. M. B. (2023). Small-scale mining and child labour in Kolwezi, Democratic Republic of Congo. Journal of African Studies and Development, 15(4), 69–83. https://doi.org/10.5897/JASD2023.0679
- Cossa, H., Dietler, D., Macete, E., Munguambe, K., Winkler, M. S., & Fink, G. (2022). Assessing the effects of mining projects on child health in sub-Saharan Africa: A multi-country analysis. Globalization and Health, 18(1), 7. https://doi.org/10.1186/s12992-022-00797-6
- Nkuba, B., Zahinda, F., Chakirwa, P., Murhi, I., de Haan, J., & Bashwira, M.-R. (2019). L’or artisanal Congolais: Analyse Socio-économique et de l’utilisation du mercure. Centre d’Expertise en Gestion du secteur Minier et Agence Congolaise de l’Envrionnement.
- HRW. (2022, July 14). Child Labor and Human Rights Violations in the Mining Industry of the Democratic Republic of Congo: Testimony of Ida Sawyer at the Tom Lantos Human Rights Commission. Human Rights Watch. https://www.hrw.org/news/2022/07/14/child-labor-and-human-rights-violations-mining-industry-democratic-republic-congo
- Reilly, E., Serlemitsos, E., & Bilakwate, J. S. (2024). Key Considerations: Child Engagement in the Context of Disease Outbreaks in Eastern and Southern Africa – Infographic. Institute of Development Studies. https://doi.org/10.19088/SSHAP.2024.006
- Institut national de sante publique. (2024). Epidémie de Mpox en Republique Démocratique du Congo. Données de la semaine épidémiologique 30, 2024 Période: 22 – 28 Juillet 2024 (No. 27).
- WHO. (2021). Gender and health emergency response: A guide for public health agencies.
- Interview with Emilienne Itonga, President of IASFM. (2022). [Personal communication].
- Issahaku, G. R., Fischer, H.-T., Appiah-Brempong, E., Opoku, D., & Hanefeld, J. (2024). Strategies to foster community engagement for epidemic and pandemic preparedness and response in sub-Saharan Africa: A scoping review protocol. BMJ Open, 14(6), e082757. https://doi.org/10.1136/bmjopen-2023-082757
- UNHCR, & UNFPA. (2021). Operational Guidance: Responding to the Health and Protection Needs of People Selling or Exchanging Sex in Humanitarian Settings. UNFPA, UNHCR. https://doi.org/10.18356/9789214030942
- Lillie TA, Persaud NE, DiCarlo MC, Gashobotse D, Kamali DR, Cheron M, Nishimoto L, Akolo C, Mahler HR, Au MC, Wolf RC. (2019). Reaching the unreached: Performance of an enhanced peer outreach approach to identify new HIV cases among female sex workers and men who have sex with men in HIV programs in West and Central Africa. PLoS One, 14(4), e0213743. https://doi.org/10.1371/journal.pone.0213743. PMID: 30943205; PMCID: PMC6447144.
Authors: This brief was written by Marie-Rose Bashwira (Centre of Research and Expertise on Gender and Development-Institut Supérieur de Développement Rural, CREGED-ISDR), Isidore Murhi Mihigo (Centre d’Expertise en Gestion Minière and Laboratoire d’Economie Appliquée au Développement, Université Catholique de Bukavu) and Diane Duclos (London School of Hygiene and Tropical Medicine).
Acknowledgements: This brief was reviewed by Modeste Deffo (CP3 Country Programme Manager, International Federation of Red Cross and Red Crescent Societies, IFRC), Hayley MacGregor (Professor, Institute of Development Studies) and Patrick DMC Katoto (Deputy Director of the Centre for Tropical Diseases and Global Health and Associate Professor of Clinical Epidemiology and Global Health Infection, Université Catholique de Bukavu). We are also grateful to Huguette Kahindo Muluhirwa for sharing humanitarian expertise and Pasteur MBula for sharing insights on the situation. This brief was edited by Harriet MacLehose and Georgina Roche. This brief is the responsibility of SSHAP.
Suggested citation: Bashwira, M-R., Mihigo, I.M., and Duclos, D. (2024). Key considerations: Mpox, mining, and vulnerabilities of women and children in eastern DRC. Social Science in Humanitarian Action Platform (SSHAP). www.doi.org/10.19088/SSHAP.2024.037
Published by the Institute of Development Studies: August 2024.
Copyright: © Institute of Development Studies 2024. This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY 4.0). Except where otherwise stated, this permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated.
Contact: If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Juliet Bedford ([email protected]).
About SSHAP: The Social Science in Humanitarian Action (SSHAP) is a partnership between the Institute of Development Studies, Anthrologica , CRCF Senegal, Gulu University, Le Groupe d’Etudes sur les Conflits et la Sécurité Humaine (GEC-SH), the London School of Hygiene and Tropical Medicine, the Sierra Leone Urban Research Centre, University of Ibadan, and the University of Juba. This work was supported by the UK Foreign, Commonwealth & Development Office (FCDO) and Wellcome 225449/Z/22/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of the project partners.
Keep in touch
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter